Understanding Uterine Cancer: Symptoms, Risks, and Treatment Options
Early detection saves lives!
What do we know about Uterine cancer and how common is it?
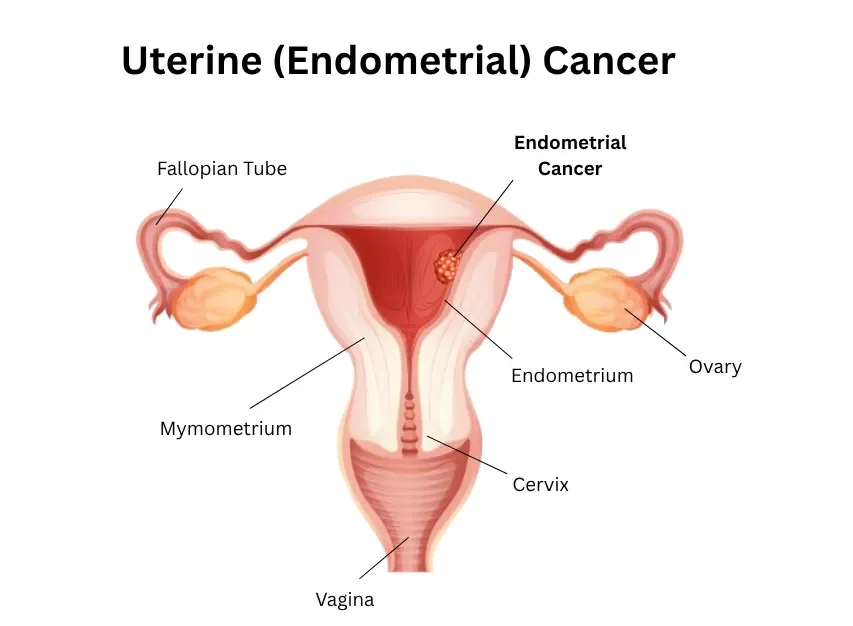
Uterus is part of the female reproductive system. It has 2 layers: outer muscle layer called myometrium and inner lining called endometrium. Cancer of the uterus occurs when cells in any part of the uterus become abnormal, grow abnormally and form a tumour.
About 3300 women in Australia are diagnosed with uterine cancer every year, and majority of them are over the age of 50. It is the 5th most common cancer in women and the most common gynaecological cancer in Australia.
Yet, despite these numbers, many women hesitate to speak up about unusual symptoms, mistaking them for normal changes. Recognising warning signs early, such as unexpected bleeding, pelvic discomfort, or unusual discharge, is crucial, because early detection dramatically improves treatment outcomes and can even be life-saving.
Get ready to be informed about the key symptoms, risk factors, and treatment options for uterine cancer, so you can take proactive steps to protect your health.
Is Uterine Cancer and Endometrial Cancer the Same?
No, uterine cancer and endometrial cancer are not exactly the same, but the terms are often used interchangeably because one is a type of the other. Uterine cancer is the broad, umbrella term for any cancer that begins in the uterus (womb). Since endometrial cancer accounts for about 90–95% of all uterine cancers, it is by far the most common type, leading to the frequent, but technically imprecise, use of the two terms as synonyms.
Types of Uterine Cancer
Uterine cancer can develop in different parts of the uterus, and the type of cancer affects both symptoms and treatment options. The main types include:
1. Endometrial Carcinoma (The Most Common)
This type accounts for approximately 90–95% of all uterine cancers and begins in the endometrium, which is the inner lining of the uterus. Endometrial cancers are further divided into subtypes, most notably:
Type I (Endometrioid Adenocarcinoma) This is the most common subtype and is typically linked to a high lifetime exposure to estrogen (often associated with obesity). These cancers are generally less aggressive, grow more slowly, and are usually diagnosed at an early, curable stage. Type II (Serous and Clear Cell Carcinomas) These are less common but are considered more aggressive subtypes. They are not linked to estrogen and are more likely to be diagnosed at a later stage because they can grow and spread more quickly.
2. Uterine Sarcoma (The Rare Type)
This type is rare, making up less than 10% of all uterine cancers, and is much more aggressive than most endometrial cancers. Sarcomas start in the myometrium (the muscular wall) or supportive connective tissue of the uterus. Key subtypes include:
How fast does uterine cancer grow?
The growth rate of uterine cancer can vary significantly depending on the type, grade, and individual patient factors.
Endometrial adenocarcinoma (the most common type) usually grows slowly, especially the low-grade forms. Many women may have early-stage disease for months or even years before symptoms appear. Serous or clear cell carcinoma (less common types) are more aggressive and can spread quickly, sometimes within a few months.
Recognising the Signs and Symptoms: Don't Ignore the Signs
The encouraging news about endometrial cancer is that it often causes symptoms early on, leading to diagnosis at a time when the cancer is highly treatable. The most common and critical symptom is abnormal vaginal bleeding.
Key Symptoms to Watch For:
Any vaginal bleeding or spotting after menopause. This is the most important warning sign and should always be investigated by a doctor immediately. Bleeding after menopause is never normal.
Irregular or unusually heavy vaginal bleeding between periods if you are still menstruating.
Very heavy periods or a noticeable, persistent change in your typical menstrual cycle.
Abnormal vaginal discharge, which may be watery, blood-tinged, or have an unusual odour.
Pelvic pain or a feeling of pressure or fullness in the lower abdomen.
The excellent news about uterine cancer is that, unlike ovarian cancer, it typically provides a clear and urgent warning sign: abnormal vaginal bleeding. Because the cancer forms in the endometrial lining, it causes this lining to shed in an unexpected way, often leading to very early detection.
Here are the critical signs and symptoms that demand a conversation with your doctor:
Symptoms for Pre- and Peri-Menopausal Women
If you are still having periods, it can be harder to spot, but look for changes in your established cycle:
Bleeding Between Periods (Intermenstrual Bleeding): Bleeding or spotting that occurs mid-cycle, not during your normal menstrual flow.
Abnormally Heavy or Prolonged Periods (Menorrhagia): A sudden, persistent, and significant increase in the heaviness or duration of your monthly bleeding that is unusual for you.
Irregular Cycles: A cycle that suddenly becomes erratic, where the timing and flow are unpredictable.
Don’t ignore the warning signs. If you have any concerns about abnormal bleeding, pelvic discomfort, or other symptoms, early consultation is key. Contact Dr. Priyanka Karine, a trusted gynaecologist, today to discuss your risks, schedule a thorough check-up.
Risk Factors: What Causes Uterine Cancer?
Uterine cancer doesn’t have a single cause, but several factors can increase a woman’s risk. Understanding these risk factors for endometrial cancer or uterine cancer can help you take proactive steps for prevention and early detection.
1. Age
The risk of uterine cancer increases with age, especially after 50.
Most cases are diagnosed in postmenopausal women, though it can rarely occur in younger women.
2. Hormonal Imbalance
Excess estrogen without enough progesterone can stimulate the endometrial lining, increasing cancer risk.
Conditions like polycystic ovary syndrome (PCOS), irregular periods, or prolonged use of estrogen-only hormone therapy can contribute.
3. Obesity
Higher body fat levels can lead to increased estrogen production, which may fuel endometrial cell growth.
Obese women are 2–4 times more likely to develop uterine cancer compared to women with a healthy weight.
4. Family History and Genetics
A family history of uterine, ovarian, or colorectal cancer may indicate a genetic predisposition.
Conditions like Lynch syndrome (hereditary nonpolyposis colorectal cancer) significantly increase risk.
5. Medical Conditions
Diabetes, hypertension, and metabolic syndrome are linked with higher uterine cancer risk.
Women with previous breast or ovarian cancer may also have an increased likelihood of developing uterine cancer.
6. Lifestyle Factors
Sedentary lifestyle, poor diet, and smoking may contribute to increased risk.
Maintaining a healthy weight, regular exercise, and a balanced diet can help reduce risk.
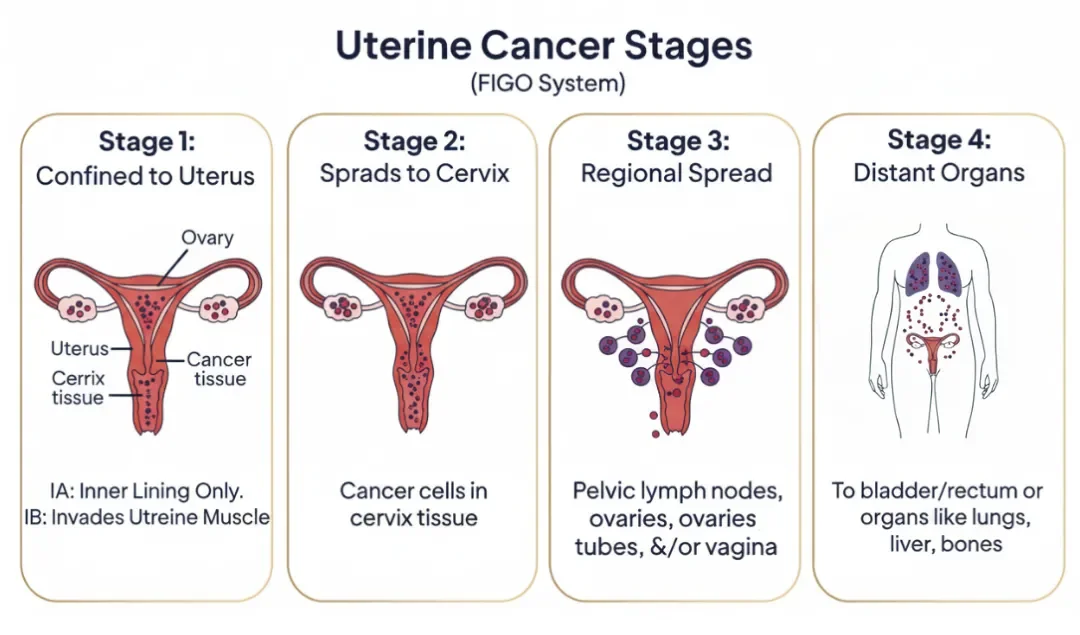
Different Stages of Uterine Cancer in Women
Uterine cancer develops in the lining of the uterus and can progress in severity depending on how far it has spread. Understanding the stages helps women and doctors identify the extent of the disease and anticipate possible symptoms.
Stage I – Cancer confined to the uterus
At this stage, the cancer is limited to the uterus and has not spread to nearby structures.
Stage IA: Cancer affects only the inner lining (endometrium) or has invaded less than half of the uterine muscle (myometrium).
Stage IB: Cancer has invaded more than half of the myometrium but remains confined within the uterus.
Stage II – Cancer spreads to the cervix
At Stage II, cancer extends beyond the uterus to the cervix, but has not reached other pelvic organs.
Treatment typically involves surgical removal of the uterus (hysterectomy) along with the cervix, often followed by radiation therapy to reduce the risk of recurrence.
Stage III – Cancer spreads locally beyond the uterus
At this stage, cancer has spread outside the uterus but is still within the pelvic area.
Stage IIIA: Cancer invades the outer layer of the uterus (serosa), fallopian tubes, or ovaries.
Stage IIIB: Cancer spreads to the vagina or surrounding tissues (parametrium).
Stage IIIC: Cancer reaches the pelvic and/or para-aortic lymph nodes, indicating regional spread.
Stage IV – Cancer spreads to distant organs
This is the most advanced stage, where cancer has spread to distant parts of the body.
Stage IVA: Cancer invades nearby organs like the bladder or rectum.
Stage IVB: Cancer spreads to distant organs such as the lungs, liver, or distant lymph nodes.
What is a Diagnosis of Uterine Cancer?
Diagnosing uterine cancer involves a combination of medical history, physical examination, imaging, and laboratory tests to confirm the presence of cancer and determine its stage. Early detection is key to effective treatment. Here are the key diagnostic procedures for uterine cancer:
1. Initial Evaluation
Medical History and Physical Exam: The doctor will discuss your symptoms, risk factors, and family history. A pelvic exam is performed to check the uterus, ovaries, and rectum for any abnormal lumps or changes.
Transvaginal Ultrasound (TVUS): This is often one of the first tests. A small probe is inserted into the vagina, which uses sound waves to create a picture of the uterus. It is used to measure the thickness of the uterine lining (endometrium).
2. Tissue Sampling (Biopsy) to Confirm Cancer of the Uterus
A tissue sample is the only way to definitively diagnose uterine cancer.
Endometrial Biopsy:This is the most common and often first step. A thin flexible tube (pipelle) is inserted through the cervix into the uterus, and a small amount of tissue is suctioned from the lining. This procedure can often be done in the doctor's office.
Pathology: The tissue sample from the biopsy is sent to a lab where a pathologist examines the cells under a microscope to confirm if cancer is present, determine the type (e.g., endometrioid, serous), and assign a grade (how aggressive the cells look).
3. Imaging Tests for Staging
If cancer is confirmed, additional imaging is often performed to determine the stage of the cancer (how far it has spread).
Ultrasound: Often the first step to assess the uterus and endometrium thickness.
MRI (Magnetic Resonance Imaging): Helps determine depth of invasion into the uterine wall.
CT (Computed Tomography) Scan: Checks for spread to lymph nodes or other organs.
PET Scan: Detects cancer cells that may have spread beyond the pelvis.
Take control of your health. Schedule your professional imaging today with Dr. Priyanka Karine and take the first step towards early detection.
What is the Treatment for Uterine Cancer?
The treatment for uterine or endometrial cancer depends on the stage of the cancer, the type and grade of tumour, and the patient’s overall health. Treatment may involve surgery, radiation, chemotherapy, hormone therapy, or targeted therapy, sometimes in combination.
Surgery
Surgery is the most common treatment for uterine cancer, especially when it is caught early. The main procedure is a hysterectomy, which removes the uterus, and sometimes the cervix, ovaries, and fallopian tubes. Doctors may also remove nearby lymph nodes to check if cancer has spread. Surgery can be done through open surgery or minimally invasive methods depending on the case.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be given after surgery to prevent cancer from coming back, or as the main treatment if surgery isn’t possible.
Chemotherapy
Chemotherapy uses strong medicines to kill cancer cells. It is usually given for advanced cancer or when it has spread beyond the uterus. Common drugs include carboplatin and paclitaxel. Chemotherapy may cause side effects like nausea or fatigue, but it helps control cancer and prevent it from spreading.
Hormone Therapy
Some uterine cancers grow because of hormones like estrogen. Hormone therapy uses medications to block these hormones or slow cancer growth. It is often used for slow-growing cancers or for patients who cannot have surgery.
Targeted Therapy and Immunotherapy
These are newer treatments for advanced uterine cancer. Targeted therapy attacks specific parts of cancer cells, while immunotherapy helps the body’s immune system fight the cancer. They are usually used when other treatments are not enough.
Uterine cancer can often be cured, especially if it is detected early. When the cancer is still confined to the uterus, surgery alone or with radiation can remove it completely, giving a very high chance of recovery. Even if the cancer has spread to nearby tissues, treatments like surgery, chemotherapy, or radiation can still be effective.
Final Thoughts!
Unlike many cancers, uterine cancer often signals its presence early through clear symptoms, giving you a crucial window for intervention. Knowing the symptoms, understanding the stages, and being aware of treatment options empowers you to take control of your health. Regular check-ups and paying attention to warning signs like abnormal bleeding or pelvic pain are essential.
Don’t wait for symptoms to worsen, your well-being deserves prompt attention. For expert guidance, accurate diagnosis, and comprehensive imaging services, book an appointment with Dr. Priyanka Karine today and take charge of your health with confidence.
The content provided in this blog is for informational and educational purposes only and is not intended as medical, legal, or professional advice. While we strive to provide accurate and up-to-date information, it should not replace consultation with a qualified professional. Always seek the advice of a licensed healthcare provider or Dr. Priyanka Karine regarding any questions or concerns you may have.